Inhalative Sedation
Informative and target level-controlled
Benefits of inhalative sedation with VA
Since years there have been efforts to bring volatile anaesthetics like Isoflurane, Sevoflurane or Desflurane from the OR to the ICU. With the intention to use their sedative effects for intensive care patients. Reason for the efforts where the extremely short context-sensitive half-lives (see figure) in comparison to prominently used intravenous sedatives. These extremely short half-lives provide an excellent controllability which makes the volatile aesthetic agents predestined for continuous sedation.
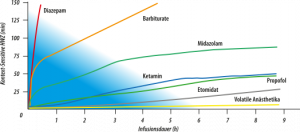
Comparison of Context sensitives half-lives
The volatile agents' metabolisation rate is low. Active metabolites are not generated during metabolisation. There is no enzyme induction. From decades and millions of cases used in, volatile anaesthetics are known to have hardly any toxicity in clinical relevant dosing. Volatile anaesthetics are also known from the OR for their excellent sedation quality in all sedation stages up to deep narcosis.
Nummerous studies show the benefits of volatile anesthetics in comparison to Propofol and Midazolam with regards to: wake-up, times, vigilance, controllability, and undesires side effects. Meiser and Laubenthal report shortend wake-up phases, missing respiratory depression and less impact on intestinal motility, providing the ability for an earlier enteral feeding progress. (Meiser und Laubenthal 2005). Mesnil et al. showed an improved wake-up quality with withdrawal syndroms after stopping the sedation with volatile anesthetics. Also a decreased morphine consumption after extubation was reported. (Mesnil et al. 2011, Sackey et al. 2005). A central statement is that the time to extubation after sedation with all volatile anesthetics is significantly shorter than with Midazolam and/or Propofol. Same for the time to react on verbal commands.
Volatile anesthetics are the almost ideal sedatives since even long-term use of volatile anesthetics does neither lead to tolerance development nor to ceiling effects or interactions with other drugs. After termination of the application the occurrence of withdrawal delir is rare.
A huge benefit in comparison to intravenous substance is the ability of continuous estimation of the current sedation depth. With intravenous sedative drugs, sedation depth can be monitored by EEG surrogates which are technically difficult and subject to errors. With volatile anaesthetics, a simple but precise and valid statement to current sedation depth is possible via the expired concentration of volatile anaesthetics (Avidan et al. 2008, Kreuer et al. 2007, Servin and Billard 2014). This opportunity is used during anaesthesia in the OR since decades and just requires a monitor for the continuous measurement of the end-tidal volatile anaesthetic agent concentration. This concentration corresponds with the anaesthetic agent concentration in the alveoli and - thus - corresponds almost to the concentration in arterial blood of the patient (Eger et al. 1965, Michael 2006).
Beside shorter wake-up times (Jung et al. 2008, Sackey et al. 2004) and shortened time to extubation (Hanafy et al. 2005), also the cardioprotective effects of volatile anaesthetics are known for years (Kehl et al. 2004, Schlack et al. 2006). The coronary bypass procedure and recanalization after acute myocardial infarct are common examples für hypoxia and reoxygenation. Volatile anaesthetics are said to provide distinct advantages in pre and post conditioning. An Italian study showed an association of volatile anaesthetics with signifactly lower troponin levels in bypass surgery procedures than with i.V. sedatives (Guarracino F et al. J Cardiothor Vasc Anesth 2006; 20: 477-483). The patients were hemodynamically more stable (less inotropic needs). The postoperative length of stay was shorter in comparison to intravenous sedated patients. In particular, fewer patients had to be hospitalized for more than 7 days.
A Swiss study investigated the postoperative application of volatile anaesthetics (Steurer MP et a. Crit Care 2012: 16: R191). Patients received an intravenous narcosis and were sedated with either intravenous or inhalative substances during weaning in the intensive care ward (4-6 hours). Also, this late post-conditioning long after reoxygenation resulted in significantly lower cardiac bio-markers.
Guerrero Orriach et al. combined Sevoflurane and Propofol with three groups (Sevoflurane intra- and postoperative, Sevoflurane intra- and Propofol postoperative as well as Propofol intra- and postoperative) (Guerrero Orriach JL et al. J Crit Care 2013; 28: 879.e13-879.e18). Patients receiving only Sevoflurane had significantly lower troponin levels compared to the patients in the other two groups. The left ventricular function marker NT-pro BNP was also lower with Sevoflurane after 24 and 48 hours.
A large retrospective comparison from Scandinavia with over 10.000 patients with Sevoflurane and Propofol showed a comparable 30-days mortality and myocardial infarction incidence (Jakobsen CJ et al. J Cardiothor Vasc Anesth 2007; 21: 664-671). However, Sevoflurane patients had more frequent ventricular fibrillation, while propofol patients had more frequent arrhythmias of other causes. In a Spanish study with 37 Propofol administered vs. 36 Sevoflurane patients (intra- and postoperative), were no differences found with regards to cardial biomarkers and intropic needs (Soro M et al. Eur J Anaesth 2012; 29: 561-569). Based on these studies there are explicit recommendations in the guide lines: "The use of volatile anaesthetics may be beneficial in hemodynamically stable and cardiac compromised patients" (Evidence level B, class II a) (Fleisher LA et al. Circulation 2007; 166: 1971-1996).
